Did you know that improper repositioning causes nearly 40% of caregiver back injuries? When assisting someone in a wheelchair, using the wrong technique doesn’t just risk your health—it can create serious pressure injuries for the person you’re helping. Pressure ulcers develop in as little as two hours when someone remains in one position too long, making proper repositioning not just helpful but medically essential.
This comprehensive guide delivers the exact step-by-step methods healthcare professionals use to safely adjust seated positions without causing strain or discomfort. You’ll learn how to read body signals that indicate repositioning is needed immediately, discover which equipment makes the process 70% easier, and master techniques that protect both you and the wheelchair user from preventable injuries.
Locking Wheelchair Brakes Properly Before Any Movement
Before touching the person, securing the wheelchair is non-negotiable for safety. Many accidents happen because caregivers skip this simple step when they’re rushed. Always engage both brakes simultaneously using a firm downward press until you hear the distinct click—don’t just rest your foot on the lever.
Identifying When Footplates Pose a Hazard
Footplates that haven’t been properly adjusted create tripping risks during repositioning. Check that feet rest flat without dangling, then swing them completely out of the way. For individuals with limited leg control, gently secure feet with non-slip straps before beginning any movement to prevent sudden kicking that could throw you off balance.
Recognizing Medical Equipment That Restricts Movement
IV poles, oxygen tanks, and catheter bags require special handling during repositioning. Always trace tubing paths before moving the person to avoid accidental dislodgement. Position yourself so these devices remain visible throughout the process, and keep emergency scissors within immediate reach in case of entanglement.
Positioning Aids That Reduce Friction During Movement

Slide sheets aren’t just helpful—they’re essential for safe repositioning. These low-friction fabrics allow you to shift body weight with minimal effort, reducing strain on both caregiver and wheelchair user. When properly positioned under the person’s hips, they cut resistance by up to 90%, making even larger individuals manageable with proper technique.
How to Position Gait Belts for Maximum Safety
A properly secured gait belt gives you stable handholds without grabbing clothing that might slip. Place it snugly (but not tight) around the waist, with the buckle positioned to the side—never directly in back where it could dig into the spine. Always check that clothing isn’t bunched underneath, which creates pressure points during movement.
Selecting the Right Pressure Relief Cushion
Not all wheelchair cushions serve the same purpose. Memory foam works well for occasional users but can trap heat for those sitting full-time. Gel cushions provide excellent pressure distribution but require careful positioning to prevent sliding. For high-risk individuals, alternating air cushions automatically redistribute pressure but need regular maintenance checks.
Two-Person Repositioning Method for Maximum Safety
This technique requires precise coordination but protects both parties from injury. Person A stands behind the wheelchair, placing one hand on each shoulder blade, while Person B positions themselves in front with knees bent and hands supporting under the thighs. The key is moving as a single unit—never let one person start before the other.
Synchronizing Movement Without Verbal Cues
In noisy environments or with hearing-impaired individuals, establish clear visual signals. A gentle shoulder tap from Person A indicates readiness, followed by a three-second countdown using raised fingers. This eliminates confusion while maintaining the critical timing needed for safe movement.
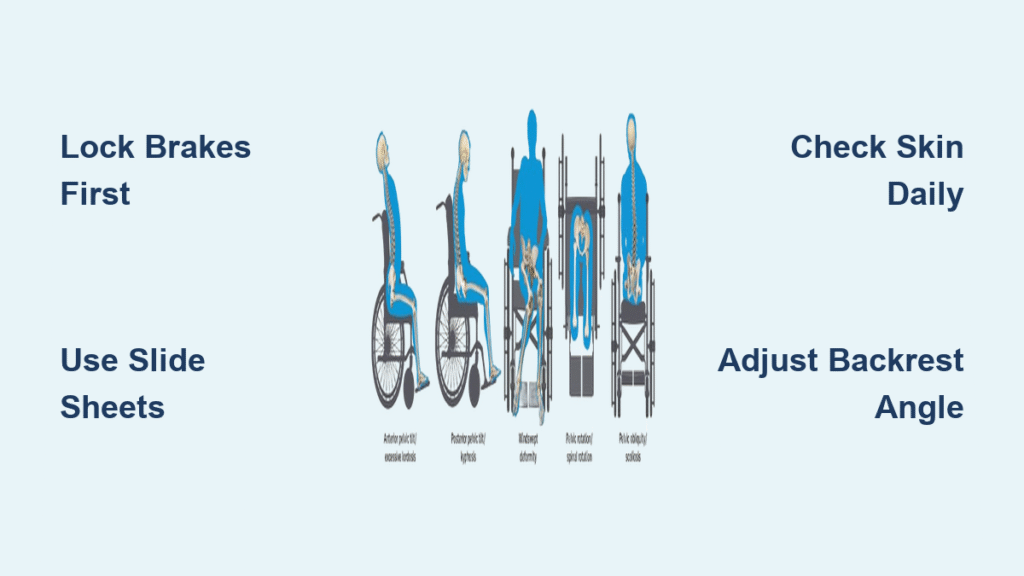
Checking Proper Alignment After Repositioning
Don’t assume the job is done once the person is shifted. Verify that both sit bones rest evenly on the seat, with hips positioned all the way back against the backrest. Run your hand along the spine to check for proper alignment—any curvature indicates improper positioning that needs immediate correction.
Solo Repositioning Techniques for Caregivers Working Alone
When you must work alone, leverage the wheelchair’s design features to minimize physical strain. Tilt-in-space functionality allows you to shift weight distribution without lifting, while adjustable footrests change center of gravity to facilitate smoother movement. Always face the direction of movement to protect your back.
Using Body Mechanics for Forward Adjustments
Stand facing the wheelchair with feet in a wide base position—never twist your spine. Place your forearms under the person’s thighs just above the knees, keeping your back straight. Use your legs to drive upward while gently guiding the person backward, allowing their own slight forward lean to create momentum.
Recognizing When Solo Repositioning Is Unsafe
Certain situations demand two-person assistance regardless of your strength or experience. Never attempt solo repositioning if the person weighs more than 50% of your body weight, has recent surgical incisions, shows signs of pain during movement, or has uncontrolled muscle spasms. Your safety matters as much as theirs.
Repositioning Individuals After Hip Replacement Surgery

Post-hip surgery requires strict adherence to positioning protocols to prevent dislocation. Always keep hips higher than knees by elevating footrests, and maintain legs in slight abduction using a specialized wedge pillow. Never allow crossing of legs or extreme hip flexion beyond 90 degrees during any movement.
Monitoring for Early Dislocation Warning Signs
Learn to recognize subtle indicators of potential hip displacement. Complaints of sudden “popping” sensations, sharp pain in the groin area, or visible shortening of the affected leg require immediate medical attention. During repositioning, maintain continuous verbal check-ins about comfort levels in the hip joint.
Preventing Pressure Ulcers Through Strategic Timing
The golden rule: reposition high-risk individuals at least every 15-30 minutes. Set visual reminders you can’t ignore—phone alarms, sticky notes on the wheelchair frame, or scheduled check-ins with timers. Don’t wait for the person to report discomfort; by then, tissue damage may have already begun.
Conducting Effective Skin Inspections
Check pressure points systematically during each repositioning session. Look for non-blanchable redness (skin that stays red when pressed), unusual warmth, or changes in texture. Pay special attention to the sacrum, heels, and shoulder blades—these areas develop ulcers most frequently but are often hidden from view.
Troubleshooting Constant Forward Sliding Issues
If someone repeatedly slides forward in their wheelchair, the problem likely stems from improper seating configuration rather than resistance to repositioning. Check if the seat depth accommodates their leg length—there should be two finger-widths between the back of the knee and the seat edge. Too much space creates a “hammocking” effect that pulls the person forward.
Adjusting Backrest Angle for Better Posture
A slightly reclined backrest (100-110 degrees) often solves sliding problems by aligning with natural spinal curvature. However, don’t exceed 110 degrees for extended periods, as this increases pressure on the sacrum. Make incremental adjustments while monitoring comfort and stability.
Aftercare Checks That Prevent Complications
Immediately after repositioning, verify three critical factors: unrestricted breathing (no abdominal compression), easy access to call buttons or communication devices, and proper alignment of medical equipment. Many caregivers skip this final check, only to discover later that tubing got pinched or positioning restricts oxygen flow.
Documenting Repositioning for Better Care Coordination
Create a simple tracking system noting the time, position achieved, and any observations about discomfort or skin changes. This documentation becomes invaluable when identifying patterns—like consistent sliding after meals—which might indicate underlying issues needing medical attention.
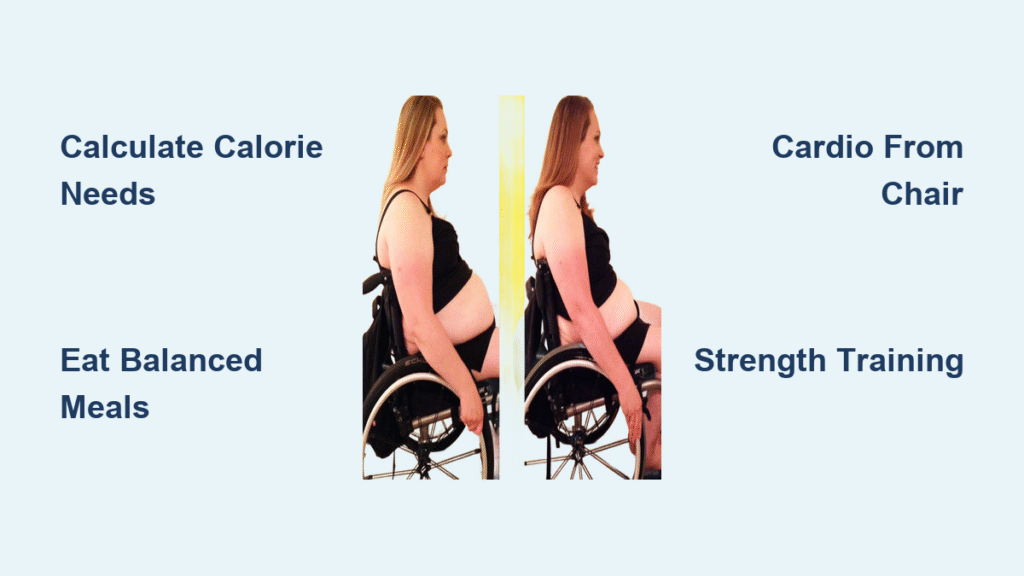
Special Considerations for Pediatric Wheelchair Users
Children’s skin is 40% thinner than adults’, making them exceptionally vulnerable to pressure injuries. Reposition smaller individuals more frequently—every 10-15 minutes—and use softer positioning aids to prevent bruising. Always involve parents in the process; children respond better to familiar voices guiding them through positioning changes.
Adapting Techniques for Growing Bodies
Children outgrow wheelchair fittings rapidly, requiring monthly seat measurements. Pay attention to signs that seating no longer fits: red marks that don’t fade quickly, complaints of numbness, or visible “perching” on the edge of the seat. Growth spurts often necessitate cushion and backrest adjustments before formal evaluations.
Bariatric Repositioning Safety Protocols
For individuals weighing over 300 pounds, mechanical lifts aren’t optional—they’re mandatory for safe repositioning. Never attempt manual transfers beyond your physical capacity, as this risks permanent injury to both parties. Use specialized bariatric slide sheets with reinforced stitching and ensure wheelchair width accommodates the person without compression.
Team Communication for Larger Individuals
When multiple caregivers assist, designate one person as the team leader who controls all movement timing. This prevents dangerous “tug-of-war” scenarios where uncoordinated efforts strain the person being moved. The leader should stand where they can see both the person and all caregivers to maintain visual oversight.
Key Takeaway: Proper repositioning combines precise technique with attentive observation—never treat it as a routine task. Start with two-person methods until you’ve mastered body mechanics, always prioritize communication over speed, and remember that small frequent adjustments prevent major complications. Your consistent attention to proper positioning preserves dignity while significantly reducing healthcare costs associated with pressure injuries. The most skilled caregivers don’t just move bodies; they create comfort through respectful, knowledgeable care that both parties experience as safe and dignified.