Struggling to navigate your home because of mobility limitations? You’re not alone—millions of Medicare beneficiaries qualify for wheelchair coverage, yet many applications get denied due to missed steps. Medicare Part B covers wheelchairs as durable medical equipment when medically necessary for indoor use, but the approval process has strict requirements that trip up 30% of applicants. Getting this wrong means paying thousands out-of-pocket or waiting months for reapproval. This guide reveals the exact sequence to secure your Medicare wheelchair coverage on the first try, including critical documentation most people overlook and cost-saving strategies for 2025.
Medicare Wheelchair Coverage Eligibility Requirements
Medicare only covers wheelchairs when your mobility issues directly impact indoor home activities—not for outdoor recreation or occasional use. To qualify, you must prove your condition prevents safe movement between essential areas like the bathroom and kitchen even with canes or walkers. Crucially, your home must have adequate doorways and safe flooring for the equipment, and you must either operate the device yourself or have consistent in-home assistance available.
Types Covered Under Medicare Part B
- Manual wheelchairs: For users who can self-propel or have reliable home assistance
- Power wheelchairs: Electric models requiring documented inability to use manual chairs
- Mobility scooters: Only covered after in-person doctor verification of safe operation
Critical Documentation You Must Provide
Your doctor must confirm in writing that your mobility limitations specifically prevent indoor home activities—not general mobility issues. This distinction causes most denials. The prescription must explicitly state how your condition affects bathroom access, meal preparation, or other essential household tasks. Without this precise language, Medicare automatically rejects claims regardless of your medical need.
Secure Your Doctor’s Wheelchair Prescription Correctly
Schedule a Mobility-Specific Consultation
Don’t wait for your annual checkup—book a dedicated appointment focused solely on mobility limitations. During this Medicare-required face-to-face visit, your physician must document how your condition affects specific indoor activities like transferring from bed to bathroom. General notes like “patient has arthritis” won’t suffice; they need phrases such as “unable to safely reach toilet without assistance due to severe knee osteoarthritis.”
Craft a Medicare-Compliant Prescription
Your prescription must include:
– Exact wheelchair type requested (manual/power/scooter)
– Medical justification tied to indoor home activities
– Confirmation of your operational capability or available assistance
– Explicit statement about home environment suitability
Pro tip: Bring this checklist to your appointment. Doctors often miss Medicare’s specificity requirements, causing 45-day reprocessing delays. A well-drafted prescription accelerates approval by 2-3 weeks.
Select Medicare-Approved Suppliers Without Overpaying
Verify Enrollment Before Committing
Only Medicare-enrolled DME suppliers qualify for coverage—using non-approved vendors means 100% out-of-pocket costs. Confirm enrollment through:
– Medicare.gov’s DME supplier directory
– Direct verification call to 1-800-MEDICARE
– Asking suppliers for their Medicare billing number
Avoid Hidden Cost Traps
Choose suppliers who “accept assignment” (agree to Medicare’s approved rates). Non-participating suppliers can charge up to 15% more—adding $300+ to power wheelchair costs. Compare prices using Medicare’s DME tool by entering your ZIP code to see:
– Medicare-approved amounts
– Supplier’s actual charge
– Your exact out-of-pocket cost
Critical warning: Legitimate suppliers never pressure you to accept unrequested equipment during unsolicited home visits. Report these scams immediately to Medicare’s fraud hotline.
Power Wheelchair Prior Authorization Process

When Authorization Is Mandatory
Medicare requires prior approval for all power wheelchairs and scooters before delivery. Your supplier initiates this by submitting your doctor’s prescription, face-to-face exam notes, and home safety assessment. Skipping this step means automatic denial regardless of medical need.
Handle Denials Immediately
If denied (typically within 10 business days), work with your doctor to:
– Add specific examples of failed indoor mobility attempts
– Include photos of narrow doorways or unsafe flooring
– Document failed trials with lower-level mobility aids
– Resubmit within 7 days to avoid restarting the process
Urgent cases: For life-threatening mobility issues (e.g., post-stroke), request expedited review—Medicare responds within 72 hours with proper documentation.
2025 Medicare Wheelchair Cost Breakdown
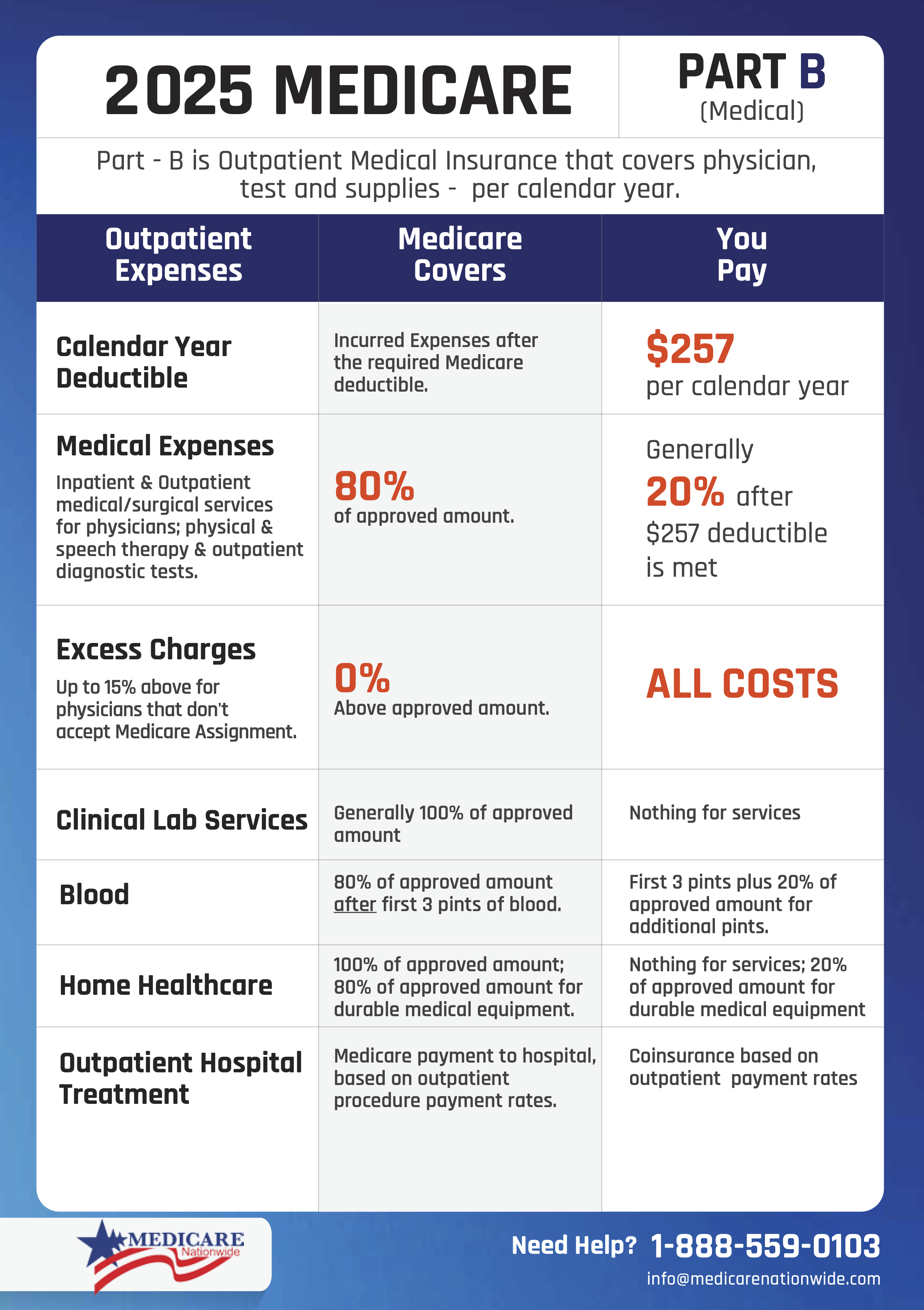
What You’ll Actually Pay
After meeting the $257 annual Part B deductible:
– Manual wheelchair: $30-$200 (20% of $150-$1,000 approved cost)
– Power wheelchair: 20% of Medicare-approved amount (varies by model)
– Monthly Part B premium: $185 minimum
Smart Rental vs. Purchase Strategy
Opt for 13-month rentals on power wheelchairs—they transfer ownership to you afterward while spreading costs. Medicare pays 80% of monthly rentals, making initial payments 60% lower than outright purchase. For example, a $5,000 power chair costs just $82 monthly during rental ($410 total before ownership) versus $1,000 upfront for purchase.
Pro tip: If enrolled in Medicare Advantage (Part C), check if your plan covers the 20% coinsurance—many include extra DME benefits for $17 average monthly premium.
Medicare Advantage Wheelchair Coverage Differences
Part C Plan Requirements
While Medicare Advantage plans must cover all Original Medicare DME benefits, they often add extras like:
– Lower or $0 coinsurance
– Expanded power wheelchair models
– Home modification assistance
– Faster prior authorization
Key limitation: You’re restricted to plan-specific supplier networks. Verify your preferred DME provider participates in your Advantage plan before applying—switching suppliers mid-process causes 30+ day delays.
Fix Denied Applications in 5 Steps
Common Denial Reasons & Solutions
- ❌ “Insufficient medical necessity”: Add activity-specific examples like “unable to reach stove without falling”
- ❌ “Home safety concerns”: Submit photos of doorway widths and flooring
- ❌ “Wrong wheelchair type”: Get revised prescription matching your functional limitations
- ❌ “Non-Medicare provider”: Switch to enrolled supplier immediately
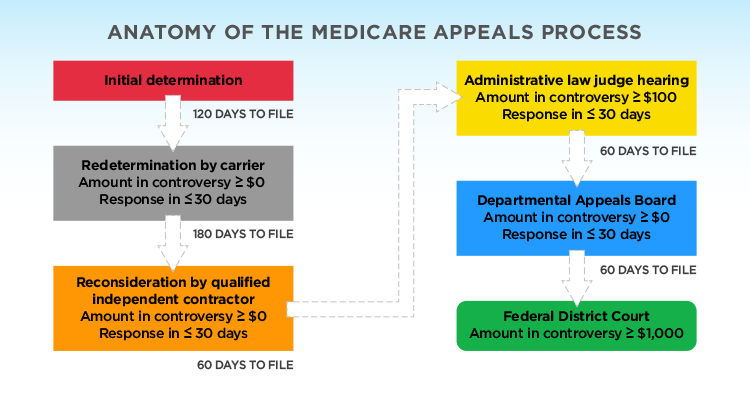
Appeal Timeline Strategy
- Day 1: Review denial letter for exact reason code
- Day 2: Contact doctor for supplemental documentation
- Day 3: Resubmit through supplier with new evidence
- Day 5: If still denied, file formal appeal with Medicare
- Day 10: Request expedited review if mobility crisis exists
Most denials reverse at Step 3 when documentation precisely addresses Medicare’s indoor-activity requirement.
Prevent Costly Application Delays
Pre-Submission Checklist
- [ ] Confirm doctor’s Medicare enrollment status
- [ ] Document specific indoor mobility failures (e.g., “fell twice trying to reach bathroom”)
- [ ] Measure home doorways (must be ≥32″ for standard chairs)
- [ ] Select supplier accepting assignment
- [ ] Initiate prior authorization before ordering equipment
Red Flags That Trigger Denials
- Doctor’s note says “patient needs wheelchair” without indoor activity details
- Prescription lists “power chair” without justifying manual chair inability
- Supplier not enrolled in Medicare
- Home assessment missing for power equipment
Time-saver: Complete home measurements before your doctor’s appointment—this speeds prescription accuracy by 50%.
Emergency Declaration Coverage Exceptions
During presidentially declared disasters (hurricanes, pandemics), Medicare temporarily:
– Waives face-to-face exam requirements
– Allows non-enrolled suppliers
– Covers outdoor mobility equipment
– Speeds prior authorization to 24 hours
Check active emergency status via:
– 1-800-MEDICARE hotline
– FEMA.gov disaster declarations page
– HHS Emergency website
Critical: These exceptions last only 60 days post-declaration—don’t assume permanent rule changes.
Post-Approval Equipment Management
Delivery & Acceptance Protocol
When your wheelchair arrives:
– Verify model matches prescription exactly
– Test operation with delivery technician present
– Confirm all accessories (cushions, trays) are included
– Note any defects before signing delivery form
Never accept equipment that doesn’t match your prescription—this invalidates coverage and makes returns costly.
Maintain Long-Term Coverage
Keep records of:
– Annual doctor recertification (required for continued use)
– Repair receipts (Medicare covers maintenance)
– Home modification photos (if applicable)
– All Medicare correspondence
Your immediate next step: Schedule that mobility-specific doctor visit today using the documentation checklist provided. Bring photos of your home’s narrowest doorways and a log of recent mobility incidents—this reduces approval time from 60+ days to under 2 weeks. With Medicare’s strict indoor-activity requirement, precise documentation isn’t just helpful—it’s your coverage lifeline. Start this process now to avoid months of painful, unsafe mobility struggles while waiting for reapproval.