Your loved one settles into their wheelchair after breakfast, ready to face the day. But as minutes turn to hours, dangerous pressure builds against their skin without movement. Pressure injuries—the silent threat lurking beneath the surface—can develop in just two hours of uninterrupted sitting. These wounds aren’t just painful; they trigger infections, hospitalizations, and life-threatening complications. The solution? A simple, evidence-based routine that prevents 95% of these injuries. Understanding how often should a person in a wheelchair be repositioned transforms caregiving from crisis management to proactive protection.
This isn’t guesswork. Global health authorities like NICE (National Institute for Health and Care Excellence) and clinical research from institutions like Ulster University have crystallized the science behind repositioning. Whether you’re a family caregiver or nursing professional, mastering these timing protocols saves skin, reduces suffering, and preserves dignity. You’ll discover precisely when to reposition based on individual risk factors, proven techniques that prevent caregiver strain, and warning signs that demand immediate action.
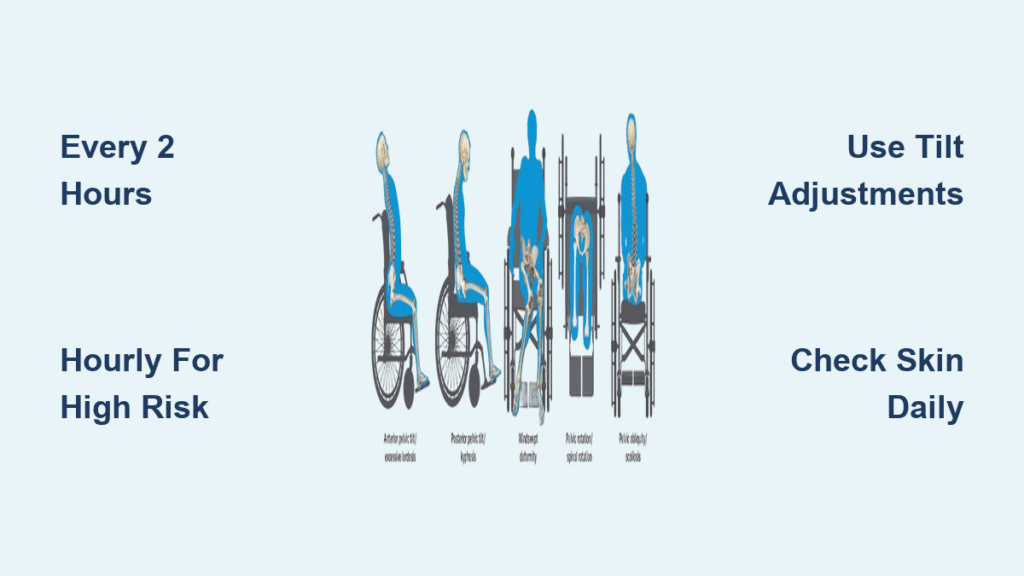
Every 2 Hours: The Non-Negotiable Minimum
Forget arbitrary schedules—reposition wheelchair users every 2 hours is the medical gold standard backed by decades of tissue oxygenation research. This critical threshold isn’t optional; it’s when blood flow to compressed tissues drops to dangerous levels. Imagine sitting on a single spot for 120 minutes straight: your skin literally begins to suffocate.
This two-hour rule applies universally—whether the user has partial mobility or complete paralysis. Even those who shift weight independently need scheduled repositioning because natural movements rarely relieve pressure across all high-risk zones. Think of it like taking vital medication: skipping a dose risks catastrophic consequences. When the clock hits 119 minutes, pressure injury prevention shifts from effective to endangered.
High-Risk Cases Requiring Hourly Repositioning

While two hours is the baseline, certain conditions demand repositioning every 60 minutes without exception. These red flags signal exponentially higher tissue vulnerability:
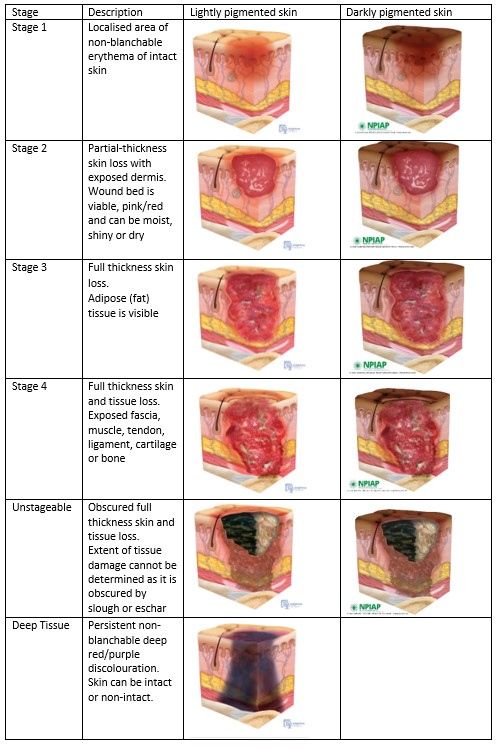
- Active pressure injuries: Any open wound, no matter how small, requires constant vigilance
- Non-blanchable redness: Skin that stays red when pressed (a stage 1 pressure injury warning)
- Complete immobility: Users unable to move any body part independently
- Incontinence: Moisture softens skin, accelerating breakdown by 500%
- Advanced age: Fragile skin in users over 65 tears more easily
- Neurological conditions: Diabetes or spinal cord injuries that impair sensation
- Poor nutrition: Malnourished skin lacks resilience under pressure
For these individuals, hourly checks aren’t “extra care”—they’re the difference between healing and life-threatening sepsis. If your loved one has multiple risk factors, treat every 60 minutes as a hard deadline.
Proven Pressure Relief Techniques That Work
Knowing how often should a person in a wheelchair be repositioned is useless without correct execution. These evidence-based methods prevent caregiver injury while maximizing tissue recovery:
For Independent Users: Quick Weight Shifts
- Side-to-side transfers: Lean fully left for 30 seconds, then right (releases ischial tuberosities)
- Forward leans: Chest-to-knees position for 30 seconds (relieves tailbone pressure)
- Armrest push-ups: Lift body 2-3 inches if shoulder strength allows (ideal for office workers)
For Assisted Repositioning: Safety-First Protocol
- Lock wheels and position draw sheet under hips
- Bend knees (never back!) during lifts
- Count “1-2-3” for synchronized movement
- Verify hips sit fully back in chair seat
- Check feet rest flat on footrests (no dangling heels)
Pro Tip: Place a pillow between knees during repositioning to prevent inner-thigh friction burns.
Research-Backed Tilt Adjustments That Save Time

Ulster University’s breakthrough study revealed a game-changing shortcut: tilting a wheelchair to maximum recline for 5 minutes reoxygenates tissues as effectively as full transfers for immobile users. This isn’t just convenient—it’s clinically proven to reduce pressure injury rates by 40% in high-risk cases.
The key insight? Pressure management requires four pillars working together: repositioning frequency, specialized cushions, tilt/recline functions, and skin monitoring. Relying solely on repositioning misses 75% of the solution. For users with tilt-in-space chairs, schedule recline sessions every 90 minutes between full repositioning to extend safe sitting time.
Home Care Scheduling Hacks That Prevent Burnout
Family caregivers often struggle with the relentless 2-hour cycle. These practical adaptations maintain safety without exhaustion:
- Mealtime integration: Reposition immediately before breakfast/lunch/dinner
- Alarm stacking: Set phone reminders labeled “REDUCE PRESSURE NOW”
- Evening wind-down: Final repositioning 30 minutes before bed
- Visitor training: Teach family to assist during visits (e.g., “Aunt Sue’s 2 PM shift”)
Long-term facilities succeed with visual tracking systems—hang a whiteboard chart showing last repositioning time. At home, use a simple sticky note on the wheelchair with colored dots (red = overdue!). Consistency matters more than clock-perfect timing—never skip a session for “just 10 more minutes.”
Warning Signs That Demand Immediate Action
During each repositioning, perform this 30-second skin scan:
| Area to Check | Danger Sign | Action Required |
|---|---|---|
| Tailbone/sacrum | Redness that doesn’t fade in 30 min | Reposition NOW + medical consult |
| Sit bones (ischial tuberosities) | Hard lumps or purple discoloration | Avoid pressure on this side |
| Heels | Blistering from footrest contact | Elevate legs immediately |
| Elbows | Scrapes from armrests | Pad armrests with foam sleeves |
Critical red flags: Broken skin, foul odor, or heat radiating from pressure points require ER attention. Don’t wait—these indicate deep tissue injury that worsens hourly.
Balancing Comfort and Medical Necessity
The hardest battle isn’t physical—it’s convincing resistant users. Wheelchair users often view frequent repositioning as infantilizing or disruptive to activities. Reframe it as empowerment: “This 2-minute shift protects your skin so you can enjoy your afternoon concert.” Offer choices: “Tilt back now or transfer to bed?” Schedule around favorite shows (“After Jeopardy, we do our pressure check”). Document preferences (“Mom prefers left-side shifts first”) to maintain consistency across caregivers.
Cost-Saving Prevention Strategies That Pay for Themselves
Treating one pressure injury costs $70,000 on average—prevention is financially smart. Invest wisely:
- $25 draw sheets: Reduce caregiver strain during transfers (prevents back injuries)
- $150 pressure cushions: Cut injury risk by 60% (Medicare often covers these)
- Free caregiver training: Local hospitals offer 2-hour workshops
- 5-minute skin logs: Prevent $10,000+ wound care costs
A quality gel cushion pays for itself after preventing just one stage 2 pressure injury. Prioritize equipment that enables independent weight shifts—this preserves dignity while reducing your physical burden.
When to Adjust Your Repositioning Schedule
Your current routine won’t last forever. Reassess these triggers immediately:
– New reddened areas after repositioning
– Weight loss exceeding 5% of body mass
– Changes in mobility (e.g., reduced arm strength)
– Introduction of new medications
Schedule professional seating evaluations every 6 months—physical therapists spot subtle alignment issues you might miss. Remember: what worked last year may now be dangerous as bodies change. Document skin responses to different positions; this data guides life-saving adjustments.
The two-hour repositioning rhythm isn’t just clinical advice—it’s a lifeline woven into daily care. By anchoring your routine to this evidence-based standard while adapting for individual risks, you transform a simple action into powerful protection. Every repositioning session is a vote for dignity, comfort, and vitality. Start today: set your timer, perform that next shift, and know you’ve just prevented a potential crisis. Your loved one’s skin—and spirit—will thank you.